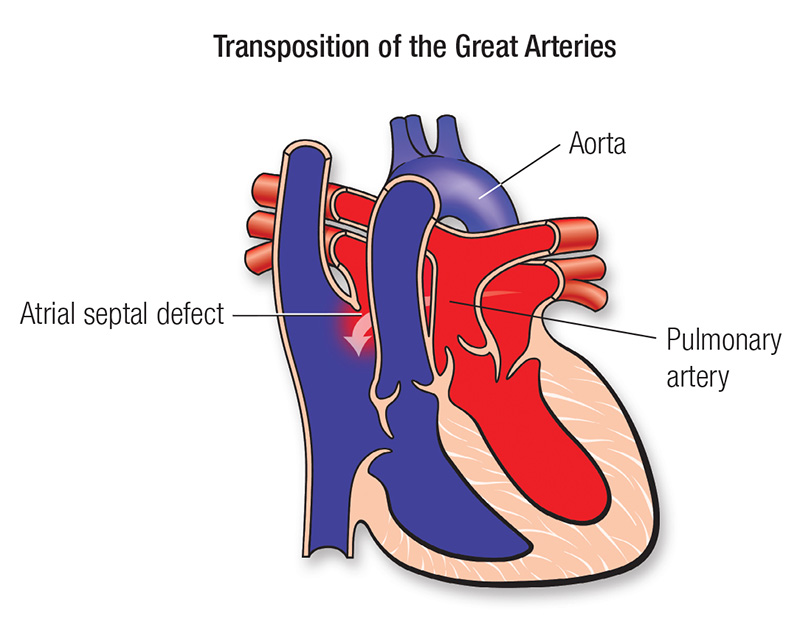
Transposition of the great arteries (TGA) is a complex congenital heart defect. In a normal heart, there are two large arteries that carry blood out of the heart. In children with TGA, these arteries are connected to the heart abnormally:
The aorta is attached to the right-sided pumping chamber (ventricle), instead of the left. The pulmonary artery is attached to the left-sided pumping chamber (ventricle), instead of the right.
The symptoms of TGA include:
Transposition of the great arteries may be diagnosed before birth, with fetal
echocardiogram (ultrasound).
Sometimes TGA is diagnosed when an infant is a few hours or days old. Less commonly, infants may not have visible symptoms for weeks or months. Paediatricians refer newborns to a Paediatric Cardiologist when they notice symptoms or abnormal values on laboratory testing such as pulse oximetry.
Diagnosis of TGA may require some or all of these tests:
Approximately one-third of newborns with TGA have extremely low oxygen levels that can harm their bodies and will require an urgent intervention. This procedure, called a balloon atrial septostomy (BAS), will take place within hours after birth. This is a life-saving procedure, which creates or enlarges a hole between the upper chambers of the heart to allow red and blue blood to mix.
All children with transposition of the great arteries will require open heart surgery to treat the defect. Without surgical repair, the overwhelming majority of patients with TGA will not survive their first year. The surgery, known as the arterial switch operation, is typically performed within a few days of birth. Surgeons reconstruct the heart so that the aorta is attached to the left ventricle and the pulmonary artery is attached to the right ventricle.
Until approximately 25 years ago, infants with transposition of the great arteries were managed by alternative surgical procedures, sometimes referred to as the “Senning” or “Mustard” operations. As a result, we don’t yet know the truly long-term effects of the arterial switch operation beyond young adulthood. It is anticipated that the overwhelming majority of children born with TGA will go on to lead healthy, productive lives.
Significant limitations of day-to-day activities, including sports, are uncommon. However, prudent physical activity after complex congenital heart surgery is recommended and is best individualized with your Childs cardiologist.
Children who have had surgical repair of TGA require lifelong care by a cardiologist. We may ask for heart tests, including ECGs, echocardiograms, cardiac MRIs and exercise stress tests. We may also evaluate your child’s cholesterol level, especially if there is a family history of adult acquired heart disease.
We will look for any narrowing where the blood vessels were sewn together. Mild vessel narrowing is usually well tolerated, but more severe narrowing may require intervention. Evaluation of long-term heart muscle function and valve function is also very important. In particular, the former pulmonary valve and surrounding tissue that now functions as the new aortic (or “neo-aortic”) valve and root on the left side of the heart can stretch over time leading to valve leakage. As with all complex congenital heart conditions, additional
surgeries may be required as the child grows. Ongoing medication use is uncommon.
