Total Anomalous Pulmonary Venous Return
Total anomalous pulmonary venous return or connection (TAPVC) is a congenital (meaning it’s present from birth) heart disease that affects the pulmonary veins.
Arteries carry blood away from the heart; veins carry it toward the heart. The pulmonary veins are very important: they carry the “red” blood that has picked up oxygen in the lungs back to the heart to be pumped out to the body. There are typically four pulmonary veins, two from each lung. Normally, they all connect directly into the heart’s left atrium (left upper chamber).
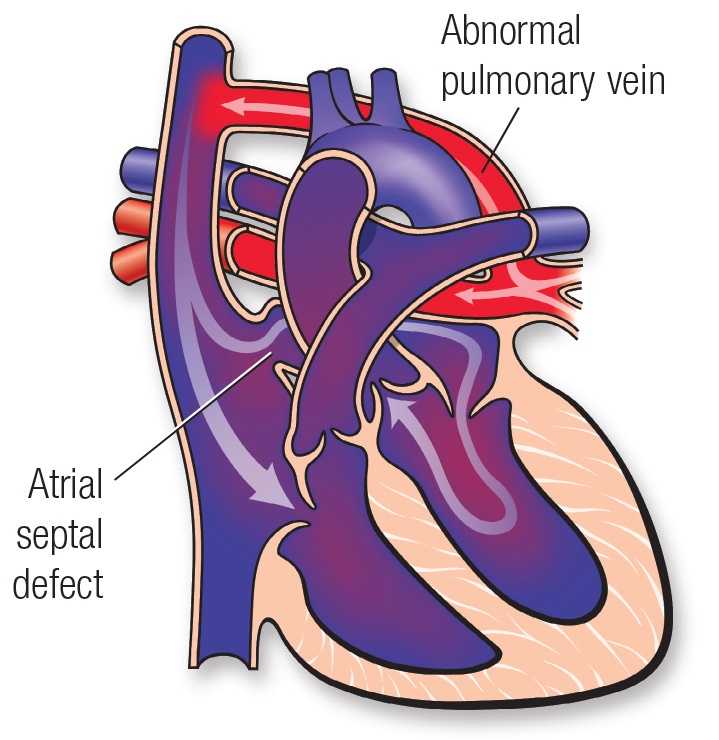
In a child born with total anomalous — which means abnormal — pulmonary venous return (TAPVR), the pulmonary veins connect to other veins and ultimately drain their blood into the right atrium. Normally, the right atrium only receives “blue” blood coming back from the body without oxygen, which then passes into the right ventricle and is pumped to the lungs. In TAPVR, the right atrium receives both “blue” blood from the body and “red” blood from the lungs.
As a result, the right side of the heart is overworked from pumping the extra blood it receives. Frequently, there is blockage to the veins that receive blood from the pulmonary veins, which causes a backup of blood in the lungs. This disrupts the normal flow of blood between the lungs and the body. Additionally, the blood leaving the heart from the body has a lower level of oxygen.
Children with TAPVR also have other heart defects. They have a hole in the wall separating the two upper chambers of the heart (atrial septal defect) and may have a patent ductus arteriosus, an extra blood vessel between the pulmonary arteries and the aorta. These heart defects can actually help the child with TAPVR survive by allowing more blood to get from the right side of the heart to the left side and out to the body. In fact, children without at least an atrial septal defect will not survive.
Generally, there are four types of TAPVR:
Supracardiac TAPVR
The pulmonary veins drain into the right atrium through the superior vena cava. The superior vena cava is a large vein that normally carries only deoxygenated, or “blue,” blood into the right atrium from the upper half of the body.
Infracardiac TAPVR
The pulmonary veins drain into the right atrium through the liver (hepatic) veins and the inferior vena cava. The inferior vena cava is another large vein that normally carries only deoxygenated blood into the right atrium from the lower half of the body.
Cardiac TAPVR
There are two types. In one, the pulmonary veins can directly enter into the right side of the heart, into the right atrium. Alternatively, the pulmonary veins can drain into the coronary sinus. The coronary sinus is a vein that normally carries deoxygenated blood from the heart muscle into the right atrium. This vein is usually very small, but becomes quite large with this abnormal amount of blood.
Mixed TAPVR
The pulmonary veins split up and drain partially to more than one of the above sites.
Total anomalous pulmonary venous return symptoms include:
The severity of TAPVR symptoms varies.
In some cases, newborns with TAPVR have difficulty breathing and quickly become very ill. This occurs when the pulmonary veins are too narrow or are obstructed at some point, and blood can’t flow from the lungs as quickly as it should.
In other cases, TAPVR is diagnosed in the first few months of life, after a child demonstrates milder symptoms such as a heart murmur or cyanosis (blue tint to skin).
Diagnosis of TAPVR may require some or all of these tests:
Total anomalous pulmonary venous return requires open heart surgery in all cases. Critically ill newborns will have surgery immediately. If the child is not critically ill, doctors may wait up to two months to perform surgery, depending on the strength of the child and the heart anatomy.
To understand the surgery, one important thing to know about TAPVR is that the pulmonary veins, despite their abnormal connections to other veins, all end in a collection or a common chamber (called a “confluence”) at the back of the left atrium. The surgeon opens the confluence and connects it to the left atrium so that the veins can drain into the left atrium. Then he or she ties off all the abnormal connections between the pulmonary veins and other veins, so that blood can follow only the path to the left atrium. The surgeon also closes the septal defects (the abnormal holes) with tiny patches or stitches, and closes the patent ductus arteriosus. As the child ages, the lining of the heart will grow over the stitches.
Because of enormous strides in medicine and technology, today most children born with total anomalous pulmonary venous return go on to lead productive lives as adults.
Children who were critically ill as newborns may have a longer road to recovery. In most cases, however, children won’t experience long-term effects. They also won’t have to remain on any medicines or limit sports.
Rarely, the pulmonary veins become obstructed later in life and additional surgery or a catheterization procedure is required. A small number of children may also experience arrhythmia (abnormal heart rhythm), which may be treated with medicines, radiofrequency ablation or a pacemaker.
Children who were born with TAPVR and had it repaired must continue to see a Paediatric Cardiologist regularly.
