Coarctation Of Aorta
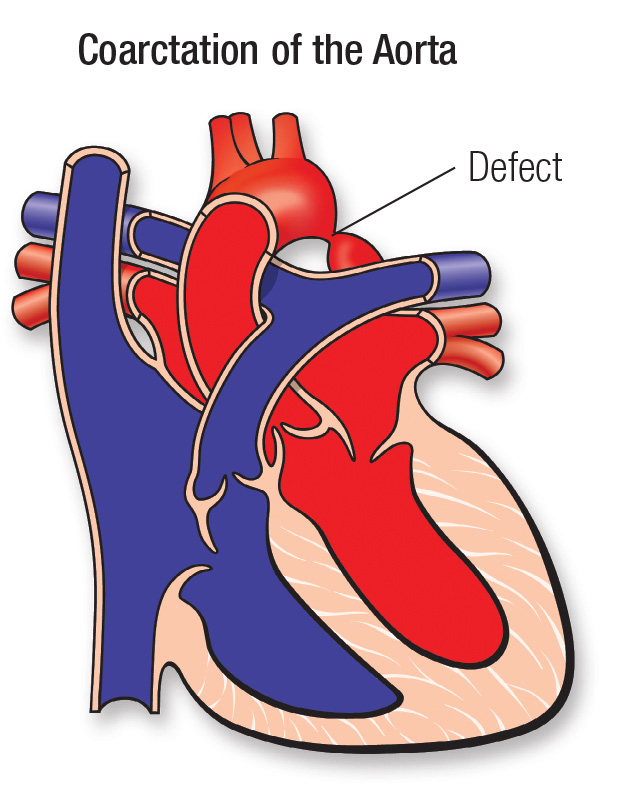
The aorta is the main artery that carries oxygenated blood out of the heart to the body. It starts at the left ventricle of the heart as one large vessel and branches out into the smaller blood vessels of the body. Arteries that deliver blood to the head, arms and other parts of the upper body branch off from the upper, ascending aortic arch. Arteries that deliver blood to the abdomen, legs and other parts of the lower body branch off from the lower, descending aorta.
In coarctation of the aorta, the portion of the aorta just after the upper-body arteries branch off is too narrow; this results in reduced blood flow to the lower body. Because of this narrowing, the left ventricle of the heart must pump much harder than normal to move blood through the aorta to the lower body. This can lead to damage to the heart (heart failure) and high blood pressure in the heart and brain. It can also damage the organs in the lower body that don’t get enough blood.
Sometimes children with coarctation of the aorta can also have a ventricular septal defect, a hole between the lower chambers of the heart, or a bicuspid aortic valve, which means the valve has two flaps instead of three.
In severe cases, coarctation of the aorta symptoms will appear within the first few days of life. The more the aorta is narrowed, the more severe the symptoms will be.
In infants where the coarctation of the aorta is severe or moderate, symptoms can include:
If the narrowing is mild, coarctation of the aorta symptoms may go unnoticed until the child
is older or even an adult. In those cases, symptoms can include:
If your infant has severe coarctation of the aorta, in most cases a doctor in the birth hospital will notice symptoms.
Milder cases of coarctation of the aorta sometimes aren’t diagnosed until the child is older. Pediatricians refer children to the cardiologist for evaluation after noticing weak lower limb pulses, if parents notice symptoms, or else if the child has high blood pressure.
Diagnosis of coarctation of the aorta may require some or all of these tests:
Echocardiogram (2D Echo): sound waves create an image of the heart
Coarctation of the aorta may require either cardiac catheterization or open heart surgery, depending on the severity of the narrowing and on other factors such as your Childs age and overall health.
Surgeons can remove the narrowed section of the aorta and then sew the ends of the aorta back together, or they can enlarge the aorta with a patch.
During cardiac catheterization, we will thread a thin tube (catheter) with a balloon on the end of it through an artery in the leg up to the heart. Then, using the catheter, we can inflate the balloon in the narrowed section of the aorta to stretch it. We might also place a stent (a stiff metal cage) in older children, to keep it open. Your child will recover from these procedures in the Intensive Care Unit at the hospital.
Because of enormous strides in medicine and technology, most children born with coarctation of the aorta go on to lead productive lives as adults.
Most children who have repair of coarctation of the aorta recover completely and won’t require additional procedures. Occasionally, the aorta becomes narrow again and balloon catheterization or surgery will be required.
We follow patients until they are young adults, coordinating care with the primary care physician. Patients will need to carefully follow doctors advice. Sometimes, these children can have persistently elevated blood pressure, despite removal of the obstruction. These children will need to take medicines to lower their blood pressure, and may need to avoid certain isometric activities, like football, weight-training and wrestling.
